Medical Malpractice: Lessons from a Plaintiff’s Lawyer
 This past Saturday our managing partner Ben Rubinowitz lectured to urologists at the Societies for Pediatric Urology SPU2021 Pediatric Urology Fall Congress held in Miami, Florida.
This past Saturday our managing partner Ben Rubinowitz lectured to urologists at the Societies for Pediatric Urology SPU2021 Pediatric Urology Fall Congress held in Miami, Florida.
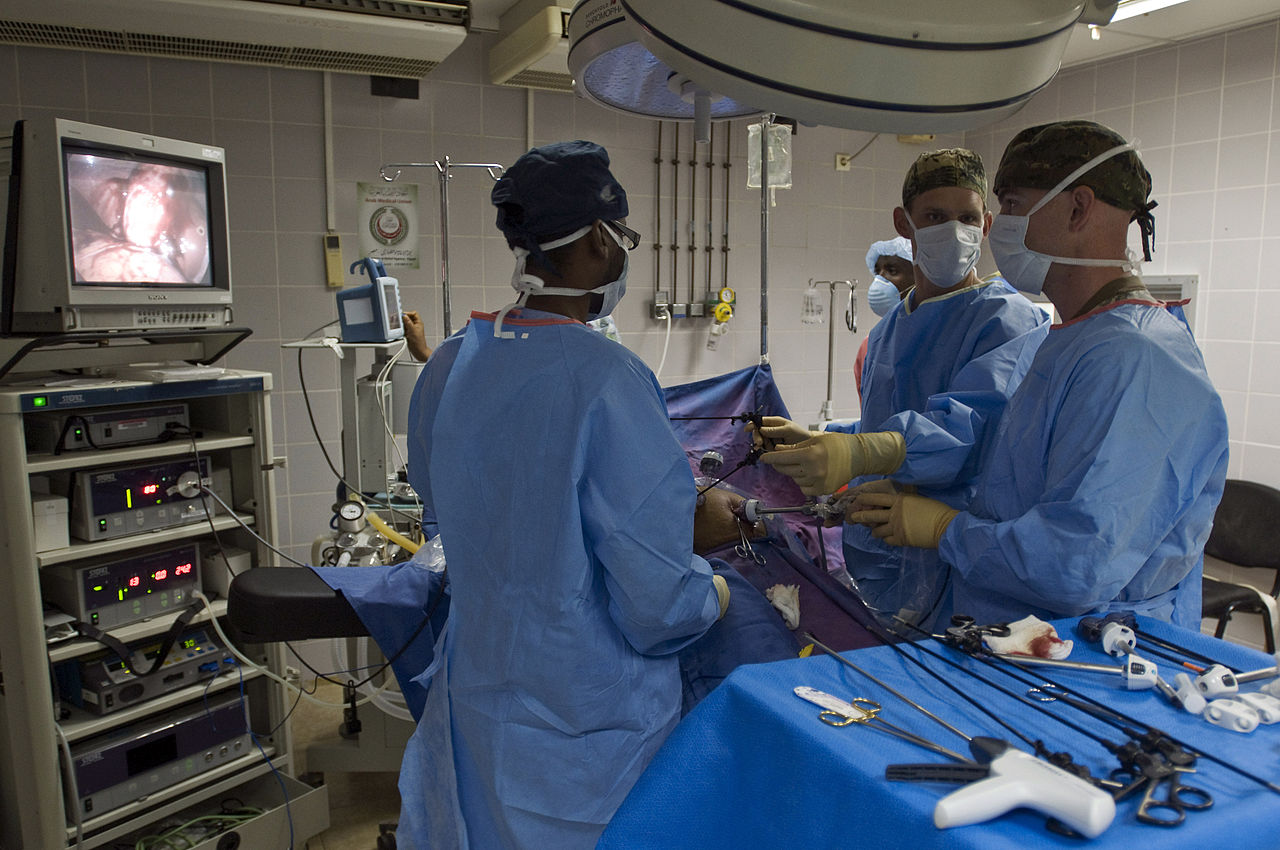
Ben presented a dynamic talk as to the pitfalls of inadequate care and the resultant harm that comes to patients when doctors fail to provide appropriate treatment. To reinforce his points, Ben cross examined doctors with regard to medical malpractice. Ben’s talk and demonstration focused on testicular torsion cases and circumcision cases gone wrong. “I consider it an honor to be invited to speak at both the Mayo Clinic and at the Pediatric Urology Fall Congress,” said Ben Rubinowitz. “ If we can prevent patients from being harmed we have all done something good — remember, we are all in this together — and no patient needs to suffer an injury that could have been prevented.”
For more than 25 years Ben has shared his expertise with physicians throughout the country. This program was attended by more than 300 urologists from across the country.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog