Among the various types of medical malpractice suffered by hospital patients, misdiagnosis accounts for approximately 10% of patient deaths. In a recent Opinion Page from the New York Times, Sandeep Jauhar, a Long Island cardiologist, wants to Bring Back the Autopsy as a weapon to fight misdiagnosis.
With the evolution of medicine and the proliferation of medical tests, autopsy doesn’t seem as essential these days as it was in the past to determine the cause of death of a patient. Before 1971, community hospitals were required to perform autopsies on 20% of their dead patients to earn their accreditation from the Joint Commission. This requirement was dropped after that date. Furthermore in 1986, Medicare considered autopsies financially draining and stopped paying for them. Now an autopsy is mostly considered by doctors as an educational tool.
Recent studies however have demonstrated that despite the medical technological advances autopsy can be a very effective manner to reduce the rate of hospital misdiagnosis. In his opinion Sandeep Jauhar suggests that Medicare and private insurers pay for them again so that financial considerations doesn’t limit their use.
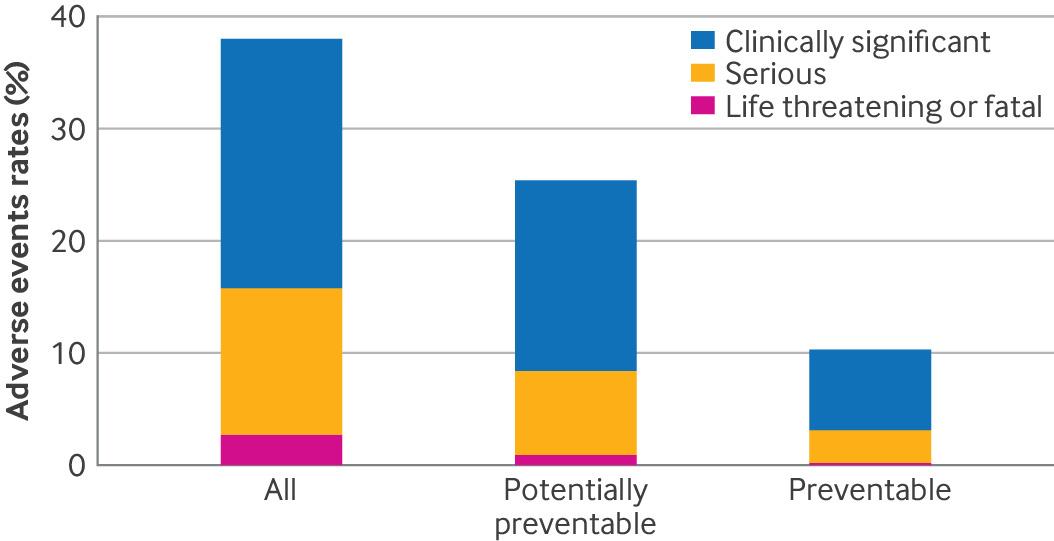 Recent findings published in the British Medical Journal (BMJ) have revealed alarming statistics about the safety of surgical care in hospitals. This extensive study, conducted across 11 U.S. hospitals, highlights the urgent need for improved safety measures to prevent adverse events during surgery. As medical malpractice attorneys, we understand the devastating impact such errors can have on patients and their families, especially when these adverse events are preventable.
Recent findings published in the British Medical Journal (BMJ) have revealed alarming statistics about the safety of surgical care in hospitals. This extensive study, conducted across 11 U.S. hospitals, highlights the urgent need for improved safety measures to prevent adverse events during surgery. As medical malpractice attorneys, we understand the devastating impact such errors can have on patients and their families, especially when these adverse events are preventable. New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog



 Medical Malpractice may have been committed on many American Africans who were previously diagnosed with hypertrophic cardiomyopathy. A recent study found that some genetic variations that were linked to this condition were indeed harmless. These specific genetic variations were found more often in black Americans than in white Americans. Therefore many patients from African descent may have been misdiagnosed or are still being
Medical Malpractice may have been committed on many American Africans who were previously diagnosed with hypertrophic cardiomyopathy. A recent study found that some genetic variations that were linked to this condition were indeed harmless. These specific genetic variations were found more often in black Americans than in white Americans. Therefore many patients from African descent may have been misdiagnosed or are still being