Are doctors failing to appropriately treat stroke patients?
More than twenty years ago, a medication was developed that can save lives and reduce the disabling impacts of a stroke. Known as tissue plasminogen activator (or “T.P.A.”), this medication is now considered the gold standard for the treatment of ischemic strokes by the American Stroke Association.
Generally speaking, there are two types of strokes that can occur—ischemic stroke or hemorrhagic stroke. An ischemic stroke occurs when there is an obstruction to one of the vessels that supplies blood to the brain. A hemorrhagic stroke occurs when a blood vessel ruptures and bleeds into the area surrounding the brain. T.P.A. can only be used to treat ischemic strokes. When timely used to treat an ischemic stroke, it can be a brain-saving treatment.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog


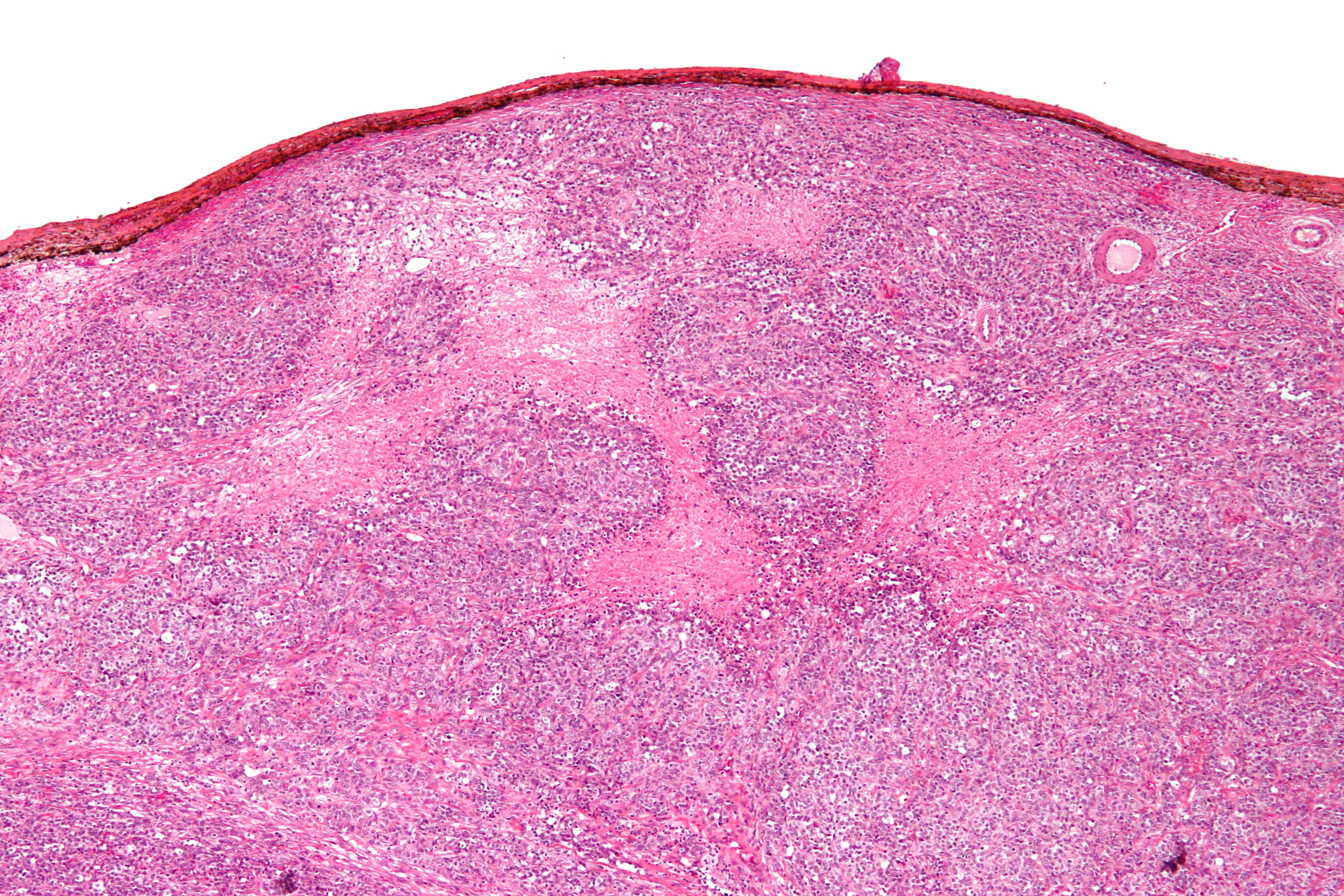
 Medical Malpractice may have been committed on many American Africans who were previously diagnosed with hypertrophic cardiomyopathy. A recent study found that some genetic variations that were linked to this condition were indeed harmless. These specific genetic variations were found more often in black Americans than in white Americans. Therefore many patients from African descent may have been misdiagnosed or are still being
Medical Malpractice may have been committed on many American Africans who were previously diagnosed with hypertrophic cardiomyopathy. A recent study found that some genetic variations that were linked to this condition were indeed harmless. These specific genetic variations were found more often in black Americans than in white Americans. Therefore many patients from African descent may have been misdiagnosed or are still being